Communicating Radiation Treatment to Patients at the University of Chicago Comprehensive Cancer Center
December 1, 2017
A remarkable 38.4% of people in the US will be diagnosed with cancer at some point during their lifetimes (Cancer.gov, May 2018), and nearly 66% of US cancer patients will receive radiation therapy (American Society for Radiation Oncology, 2015 Legislative Priorities Brief). External Beam Radiation Therapy (EBRT) is one of the most frequently used radiation treatments, yet the process is opaque and complex. Providing understandable educational material to help anxious patients and caregivers navigate the process is vital.
Current patient education material is voluminous and overwhelming. Typically written at a 12th grade reading level, with occasional stock photographs, explanation of the treatment is handed to patients in their first meeting with their doctor, a point of high emotional stress.
Communicating Radiation Treatment to Patients
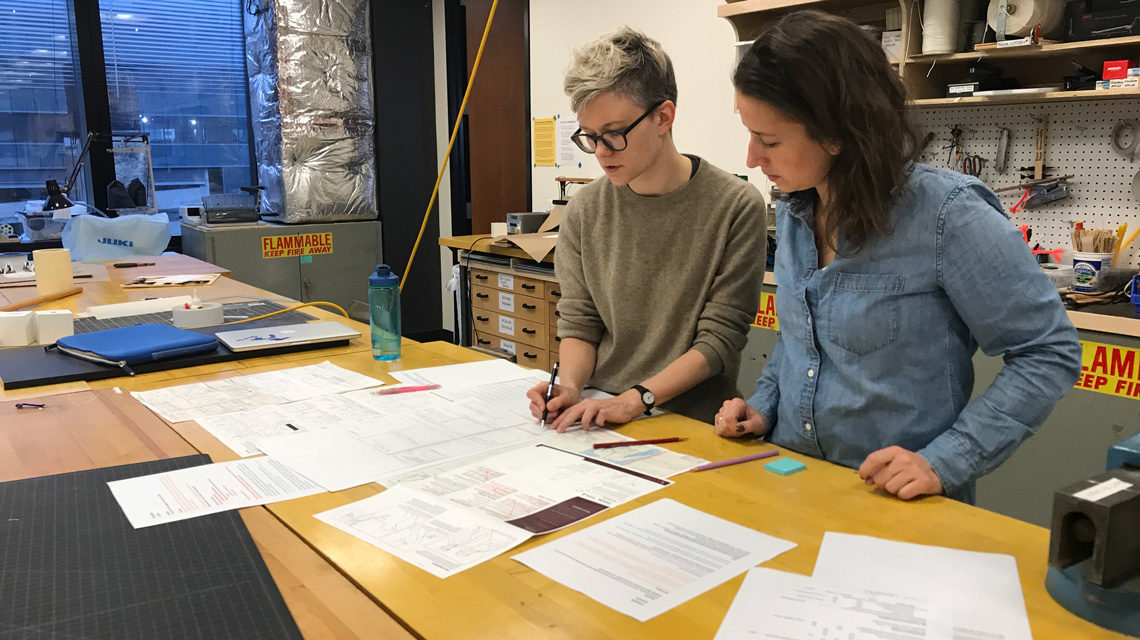
Students and faculty discuss their work with UChicago Medicine.
Synopsis
In a communication design project funded by UChicago Medicine’s Bucksbaum Institute for Clinical Excellence, an IIT Institute of Design (ID) student team partnered with Dr. Daniel Golden of UChicago Medicine to explore how visual narratives could better educate patients about radiation therapy.
- By surveying existing visual narrative styles, along with theoretical teachings from Scott McCloud, a renowned comic theorist, the team explored visual narratives, more popularly known as ‘graphic novels’ or ‘comics,’ as legitimate emerging media for serious topics in healthcare, mental illness, death, abortion, abuse, and cancer survivorship. The class learned that graphic storytelling is its own visual language that can be leveraged to display concepts such as time passage, transitions, simultaneity and projection.
- They also researched how, as healthcare delivery adopts patient-focused care, principles for public-facing communication have emerged. However, many guidelines are focused on primarily text-based materials.
- The team interviewed 26 stakeholders: patients/caregivers and medical and non-medical staff. They analyzed audio files and transcripts, extracted insights, and distilled them into design principles, ultimately creating a goal-oriented framework that streamlined the process and ensured that decisions for content representation were sound and principle-driven.
Research yielded design principles reflected in the design of a multicolor illustration-based discussion guide prototype. In easy-to-follow framing using fifth grade reading level language and simple graphic narrative-style illustrations, the team’s prototype distills what had been dozens of loose pages into one two-sided takeaway document designed to support clear communication and expectation-setting between doctor and patient.
Dr. Golden is now testing the prototype with patients. He will present “Communicating the External Beam Radiation Experience (CEBRE): A Novel Graphic Narrative Patient Education Tool” (for which ID students are listed as co-authors) to fellow radiologists at two North American forums in order to disseminate the approach, receive feedback for future iterations, and instantiate it as standard practice.
Patients have reported that the tool has made a stressful interaction easier, helps them to understand how external beam radiation works, and sets expectations for the process.
In 2018, an estimated 1,735,350 new cases of cancer will be diagnosed in the US (Cancer.gov, May 2018). Given that external beam radiation is one of the most common treatments, this communication design work could improve the experience of hundreds of thousands of cancer patients annually.
For access to the CEBRE discussion guide, which is designed to be used during the physician-patient discussion at initial consultation, visit: