External beam radiotherapy is the most common treatment for cancer, yet the process is intimidating and unfamiliar to most patients. That’s why Dr. Dan Golden, a radiation oncologist and assistant professor in the Department of Radiation and Cellular Oncology at the University of Chicago’s Pritzker School of Medicine, had the vision of a portfolio of discussion guides that could help cancer patients through it.
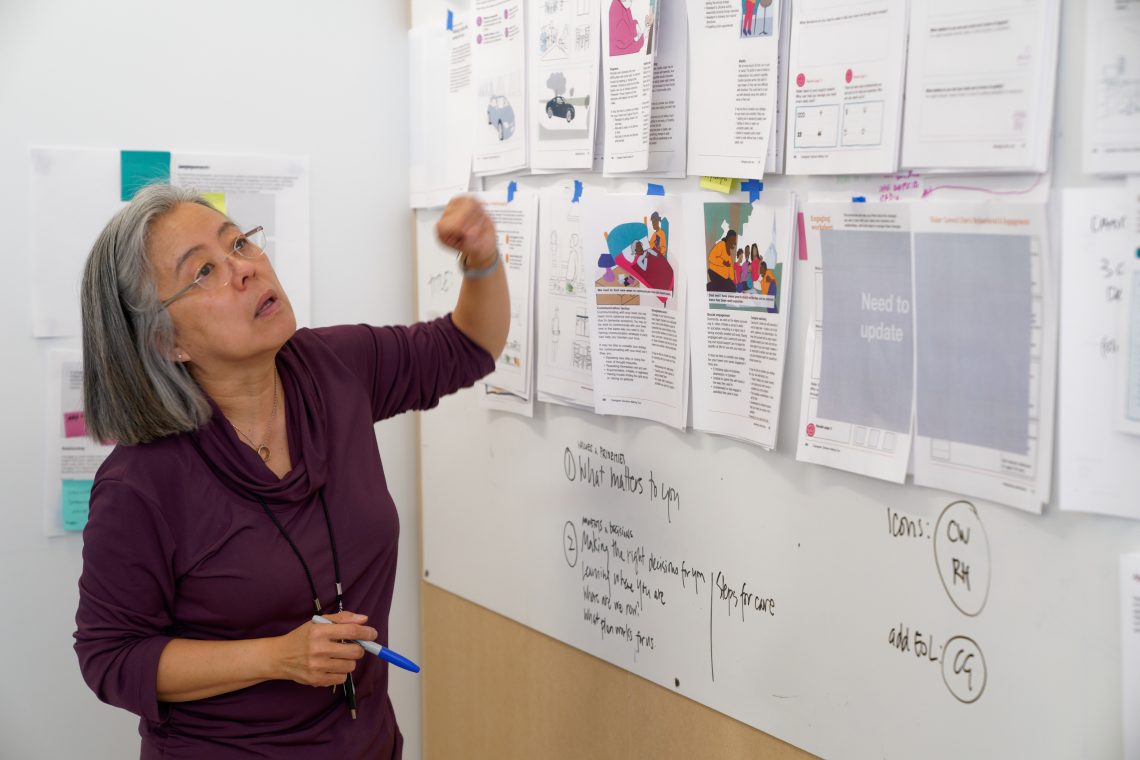
Working with ID Clinical Professor Tomoko Ichikawa and her students, and with support from UChicago’s Bucksbaum Institute for Clinical Excellence, Golden’s vision found its footing with the Communicating the External Beam Radiotherapy Experience (CEBRE) discussion guide.
The CEBRE guide uses graphic narrative and easy-to-digest information to facilitate conversations between patients (or their caregivers) and their medical care providers. The discussion guide focuses on the process of radiation treatment, which involves exposing the body to a concentrated beam of radiation to shrink a tumor.
“It helps patients to have a more concrete idea in their heads of what we’re talking about,” adds Golden. “I can show these graphic narrative images that are designed intentionally to have the right amount of detail. This helps the patient to have just the right amount of granularity to understand what’s going on, without being intimidated by it.”
Ichikawa and Golden received positive feedback from clinicians. Licensed with Creative Commons, anybody can download, print, and use the materials.
Still, a generalized discussion guide has its limits: not all cancers are approached exactly the same way, even if treated by external beam radiation.
“The 30,000-foot-view of the general treatment process is similar for treating most sorts of cancer with radiotherapy, but when you start to get into the granular details of each type of cancer you see how different they can be,” says Golden. “There are things in the general guide that are included that might not apply to all patients, and there are things that aren’t included because they’re just too specific.”
To extract more use from the original concept, and to provoke more fruitful conversations between patients and doctors, Golden and Ichikawa received two years of grant funding from the Radiation Oncology Institute to create a total of six new guides that cover the nuances of external radiation beam therapy on some of the most common cancer sites.
“What we found out in the first project is that people have these myths about that process; if a family member had cancer there’s an assumption they’ll go through the same thing,” says Ichikawa. “But every person’s situation and everyone’s treatment specifics are very unique, so we wanted to dispel that myth first and foremost.”
During the summer of 2020, the team, including two ID students—Grace Hanford (MDes + MBA 2020) and Jason Romano (MDes 2020)—created half of those guides for lung, breast, and prostate cancers. Another three guides, focusing on brain, gastrointestinal, and head and neck cancers, will be produced at a later date as well.
The CEBRE guides are characterized by their colorful illustrations of patients going through the radiation treatment process. Using principles of communication design, Ichikawa’s area of expertise, the guides visually detail the process from the very beginnings of consultation through treatment and into follow-up care. Further, the guides include areas for notes and a “My Information” section where doctors can provide details specific for the patient.
As part of their design process, Ichikawa and her students interviewed patients and caregivers as well as medical staff—including doctors, nurses, radiation therapists, social workers, and other members of the radiotherapy care team—to better understand the intricacies of the radiation treatment process and what information should be included to help ease anxiety and inform patients. For example, working with radiation oncology physicists and dosimetrists (non-patient-facing professionals who help craft the treatment plans for patients), the ID team was able to ensure the guide materials included further transparency into the process.
“Physicists and dosimetrists are the folks who devise individual treatments in terms of how big the ray should be or how often, how frequently, and how long [patients] are exposed. They’re the ones that really formulate the patient’s therapy, but they don’t ever see the patients,” says Ichikawa. “That can take a long time, a week or two even, and patients often wonder why they can’t start treatment right away. We suggested preparation activities the patients could do in the meantime so they feel more empowered, rather than being passive.”
The resulting guides, much like the original, are accessible and easy to print on a typical office printer. They fit on a single sheet of 11-by-17-inch paper and a standard color print cartridge can print the selected colors. Golden was emphatic, even during the COVID-19 pandemic, that the guides be printed on paper as he believes they’re more engaging in print format than digital.
“Often when I’m going over these guides with patients they’ll stop and ask, ‘Oh, what’s that?’ Or they’ll point at something and say, ’Oh, I see that’s how it works.’ I’ve even had patients bring the guide back or reference it at a later time following a visit,” says Golden. “Patients have even told me they take the guide home and use it to explain the radiotherapy process to their family members.”
Between the original CEBRE guide, a trio of guides made for brachytherapy (internal radiation) treatments for patients with gynecological cancers that UChicago Medicine’s gynecological oncology doctors and Ichikawa created in 2018, and the six new site specific pieces, the library of discussion guides will eventually expand to 10 pieces. Additionally, the team is actively working to translate the guides into Spanish.
All guides completed thus far are available, for free:
“I don’t want these guides to be something that only I use because that’s not worth the hundreds of hours of effort Tomoko and the students put in,” says Golden. “But if people all over the country and even the world could use them? That would be incredible.”
This story was published on IIT News.