Alzheimer’s and Dementia: Promoting Equity in Care and Outcomes
By Andrew Connor
April 20, 2020
In recent years a body of research[i] has shown that African Americans are more likely—two to three times as likely—as whites to develop Alzheimer’s disease and related dementia. Despite this disproportional effect on African Americans, there is a lack of educational materials tailored for this community.
Click to view
Gaps in access to healthcare and a lack of culturally-competent health education and caregiver resources continue to hinder the quality of care for the underserved African American population.
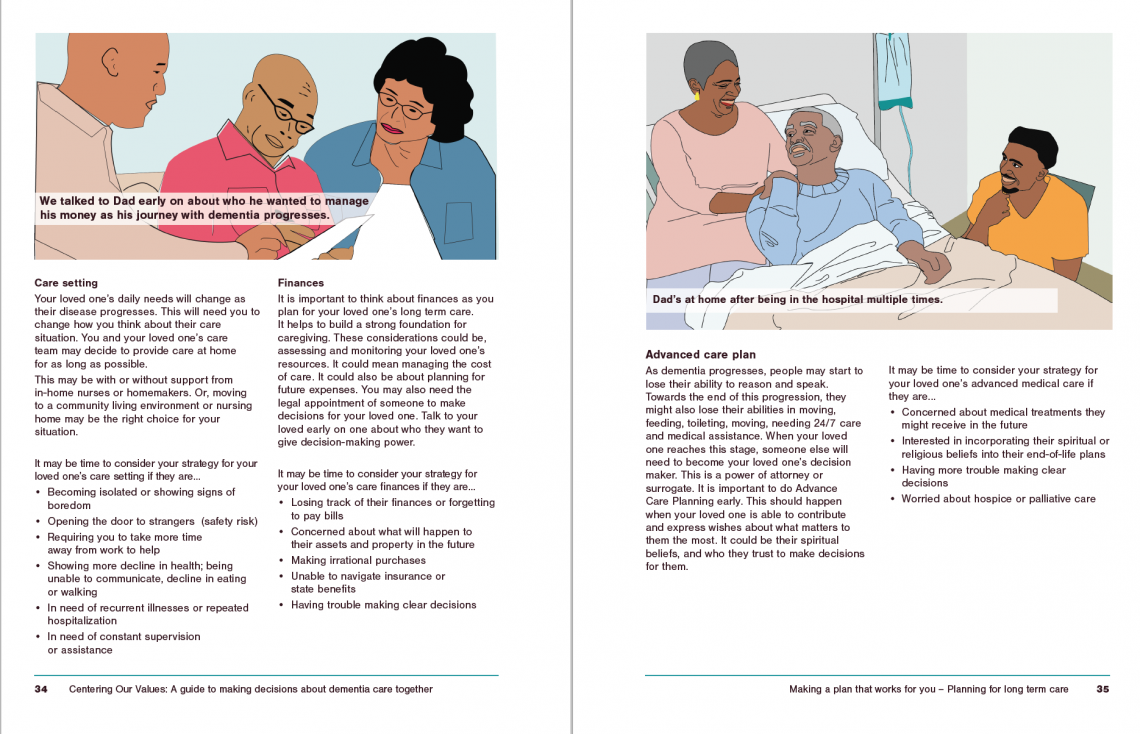
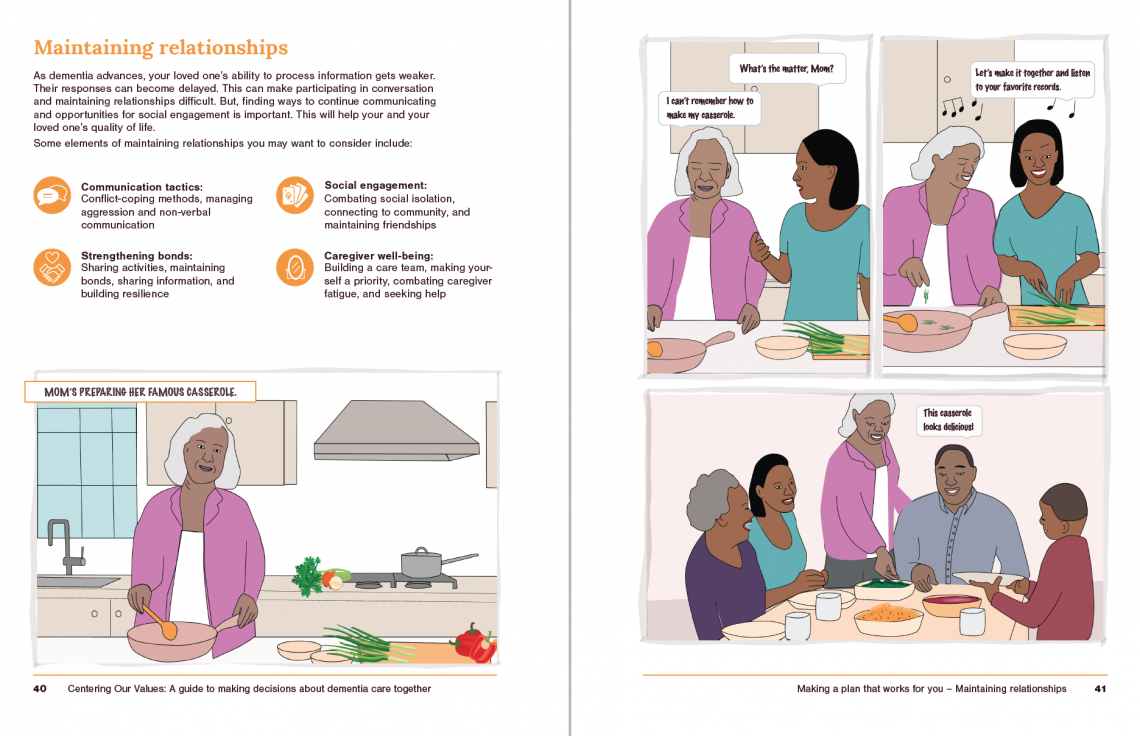
An ongoing collaborative sponsored research project between IIT Institute of Design and UChicago Medicine aims to fill that gap with the creation of a Caregiver Decision Support Tool (CDST) prototype for African-American caregivers and Alzheimer’s patients. The resulting tool is a 56-page workbook for patients and caregivers. Centering Our Values: A guide to making dementia care decisions together uses graphic narrative and standalone illustrations to show culturally appropriate solutions and care interventions.
Starting in fall 2019, Ichikawa, a group of 11 students, and Dr. Shellie Williams, an expert in geriatric and palliative care from UChicago Medicine, set out to create new materials by beginning a multi-pronged design process that started with primary and secondary research. Primary research involved interviewing 20 different types of stakeholders in the Chicago South Side community where both ID is located and UChicago Medicine serves patients, such as medical professionals, social workers, community advocates, and caregivers, to gather a wide perspective of the caregiver/patient journey.
The interview process provided insights that allowed the team to devise a litany of design principles to lead development of the tool, including that it needed to:
- Be customizable and digestible
- Help users easily understand the progression of the disease
- Make possible future circumstances foreseeable
- Emphasize the role of values in caregiving
Centering Our Values had been accepted for presentation at the American Geriatrics Society’s 2020 Annual Scientific Meeting in May 2020 and the Graphic Medicine Conference in July 2020, the latter was to focus on “Graphic Medicine in/during Trouble Times: Health, Social Justice, and Human Rights.” Both conferences have been cancelled due to the coronavirus outbreak.
Click to view
Williams’s own research has showed that caregivers lacking education about Alzheimer’s are more likely to make rash decisions in times of high stress, resulting in conflict or more aggressive end-of-life interventions for their loved ones. By creating materials that emphasize informed, values-based decisions, caregivers would have the resources to make decisions that better suit their own personalities and interests, as well as those of their loved ones.
As such, Centering Our Values encourages informed decision-making. Both caregivers and patients are given spaces to reflect on what matters most to them, and a decision-making tool based on the informed consent process allows caregivers to work through the decision-making process based on those values.
“It makes it a logical, thought-through decision, rather than an in-the-moment decision, which oftentimes can lead to something more hurtful in the end,” says Ichikawa. “By articulating the decision thought process, Dr. Williams is thinking this will empower the caregiver, rather than having power taken away from them.”
Similarly, graphic narratives and illustrations are featured heavily in Centering Our Values. In addition to providing visuals that are more representative of its African-American audience, they’re created to illustrate positive outcomes for upsetting situations that can arise with Alzheimer’s, such as memory loss, weakened interpersonal relationships, and increased dependence.
“When someone is confronted with immediate things that they have to respond to every day, they may not have the wherewithal to think through what the end result could be, and if they do, oftentimes it’s negative,” says Ichikawa. “These illustrations are sort of trying to put a positive, aspirational spin on the situation as a way to envision what possibilities might be available to them.”
The prototype that Ichikawa’s students produced in Fall 2019 will undergo focus group testing in Spring 2020 to determine the tool’s effectiveness and any changes that might need to be made in future iterations. The team hopes to make the tool readily accessible across the United States, and plans to make the graphics work in black and white for stakeholders who may not have access to a color printer.
“On this project, I felt an especially deep sense of obligation to do justice to the stories our participants shared with us, since many of them came from an emotional place. Our job as designers is often to make difficult choices in service of an ultimate goal, which is sometimes at odds with incorporating the experiences of our research participants,” says Sherrod. “In this case, our team really fought to balance providing clear information and structure with a diversity of personal experiences—ultimately, I think we came out with a good compromise.”
[i] From the abstract, published in the April 2020 issue of the Journal of the American Geriatrics Society:
Alzheimer’s disease and related dementias in the US are expected to increase from 5.3 million to 20 million by 2050 (1), and the African American subgroup is at 2–3 times greater risk for developing this disease compared to non-Hispanic Caucasians. Despite its growing prevalence, African American caregivers are often unclear on the common course of the disease, are 1.7 times more likely than non-Hispanic white populations to choose aggressive end-of-life care (2), and have a lower percentage of documentation of advance directives (2, 3).