39.5 percent of people in the US will be diagnosed with cancer at some point during their lifetimes (Cancer.gov, May 2018), and nearly 66 percent of US cancer patients will receive radiation therapy (American Society for Radiation Oncology, 2015 Legislative Priorities Brief).
External Beam Radiation Therapy (EBRT) is one of the most frequently used radiation treatments, yet the process is opaque and complex. Providing understandable educational material to help anxious patients and caregivers navigate the process is vital—current patient education material is voluminous and overwhelming.
Typically written at a 12th-grade reading level, with occasional stock photographs, an explanation of the treatment is handed to patients in their first meeting with their doctor—a point of high emotional stress.
During the research phase, patients shared with the ID team their reactions to current communications:
- “At that moment in time, it was a huge shock for me and my family. The consultation meeting was all that we had and relied on.”
- “I didn’t even look at it after going home. My daughter—yes she did. She is intelligent. But no, not me.”
- “Dr. Daniel Golden was amazing at explaining everything to me, and didn’t feel like I needed anything else other than that.”
- “There is already so much paperwork involved at the beginning and I didn’t have the energy to go through anything else, physically and mentally as well.”
To address this problem, several Institute of Design students and Associate Teaching Professor Tomoko Ichikawa first partnered with Dr. Daniel Golden of UChicago Medicine in Fall 2017 to explore how visual narratives could better educate patients about radiation therapy. This initial research project was funded by UChicago Medicine’s Bucksbaum Institute of Clinical Excellence. By surveying existing visual narrative styles and through expert presentations, the class learned that graphic storytelling is its own visual language that can be leveraged to display concepts such as time passage, simultaneity, and projection.
Following this research project, several Institute of Design students have worked on designing a series of six discussion guides, with plans to include a seventh next year. These guides are used by doctors in their first consultation meetings with patients helping them to explain external beam radiation therapy treatment for malignant and benign tumors located in the Brain, Breast, Digestive System, Head and Neck, Lung, and Prostate. We received funding from the Radiation Oncology Institute to continue this project over two years, starting in 2020.

The newest three discussion guides: Brain, Head and Neck, and Digestive System
Over Summer 2022, two ID students, Keval Parekh (MDes 2023) and Mayukhi Chacham (MDes 2023) worked again with Tomoko Ichikawa and Dr. Daniel Golden from UChicago Medicine to design the latest discussion guides for the Brain, Head and Neck, and Digestive System.
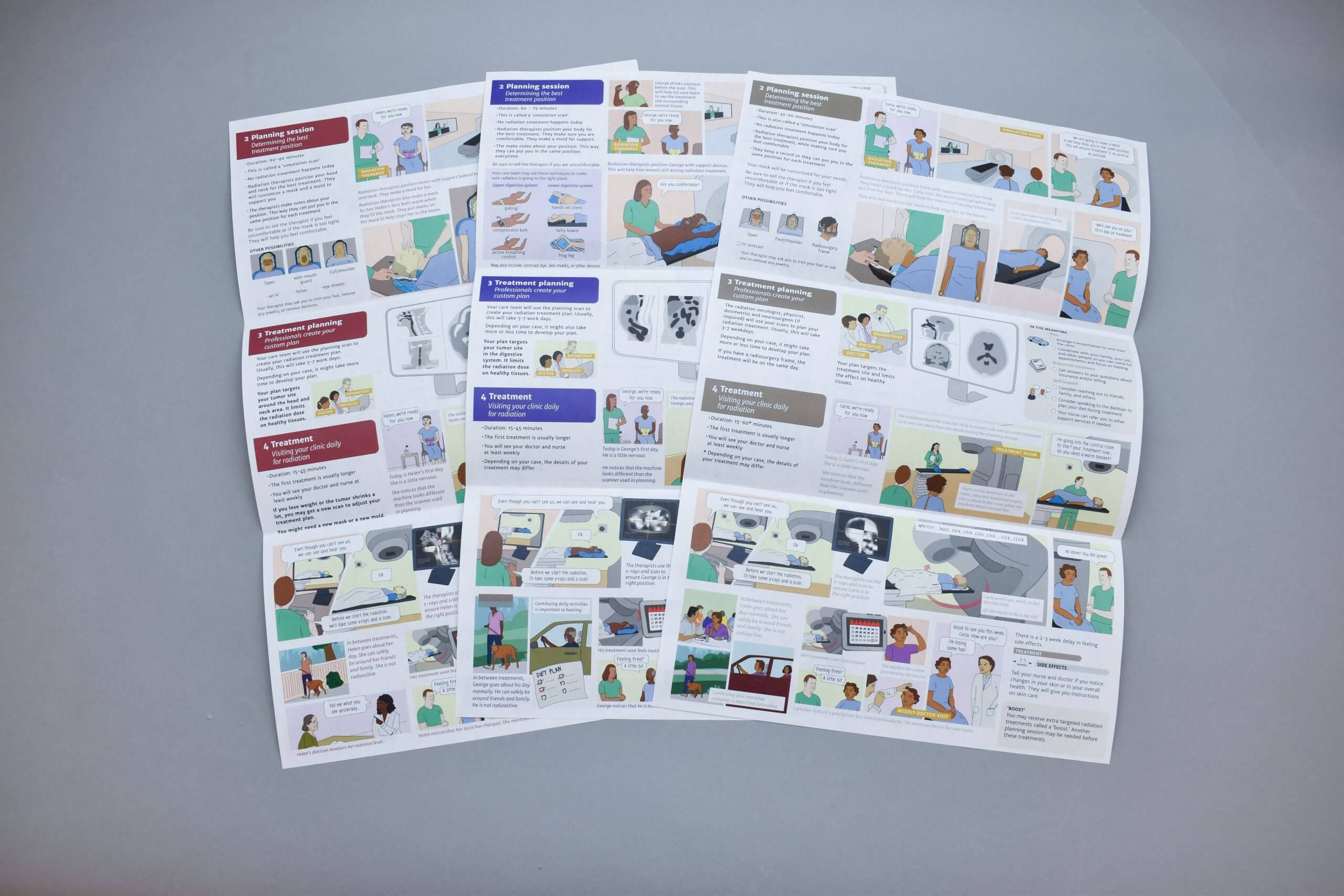
The newest three discussion guides: Brain, Head and Neck, and Digestive System
The team interviewed 26 stakeholders, including patients/caregivers, medical, and non-medical staff. They analyzed audio files and transcripts, extracted insights and distilled them into design principles, and ultimately created a goal-oriented framework that streamlined the process and ensured that decisions for content representation were sound and principle-driven.
By using sixth-grade level reading content and a graphic narrative, these discussion guides are easier to read and understand than previous educational material provided to patients. The content of the guides is broken down into different sections that divide the treatment process and describe a patient’s journey. Doctors also have the ability to write on and add to the guides in order to remind patients about special conditions or any treatment information they might have. The design decisions are patient-centered as much of the approach to designing and writing content was focused on making it easier for the patients to consume information. Also, the choice of comic characters in these discussion guides represents diversity and helps patients relate.
Patients have reported that the tool makes stressful interactions easier, helps them to understand how external beam radiation works, and sets expectations for the process. These guides visualize what’s coming next in the treatment journey, which helps patients anticipate possible needs, decreases their anxiety, and empowers them to be active participants in their treatments. The guides can also result in improved patient-physician relations and care delivery.
All discussion guides are designed and published in English, and available to download for free. They are in the process of being translated into Spanish, facilitating a wider audience and larger impact around the world.
In 2019, an estimated 1,752,735 new cases of cancer were diagnosed in the US (Cancer Data and Statistics, CDC). Given that external beam radiation is one of the most common treatments, this communication design work could improve the experience of hundreds of thousands of cancer patients annually.
For access to the CEBRE discussion guides, which are designed to be used during the physician-patient discussion at the initial consultation, please visit: